A 28-year-old man L.H.N who presented City International Hospital, complaining of progressive and headaches, nausea, and vomiting due to Food Poisoning,. Brain MRI At City International Hospital, a complex AVM (an abnormal tangle of vessels in the brain) was found.
21 March 2019, arrived at City International Hospital, a young 28-year-old L.H.N had experienced worsening neurologic symptoms of Fever, headache, nausea, and vomiting. Learning historical records of the patient, before City International Hoospital he went to several hospitals and got diagnosed with a first episode of with brain bleed and was prescription drugs to control blood pressure. Though, the patient still suffered from insomnia due to multiple headaches, he was taken to the International City Hospital for urgent help.
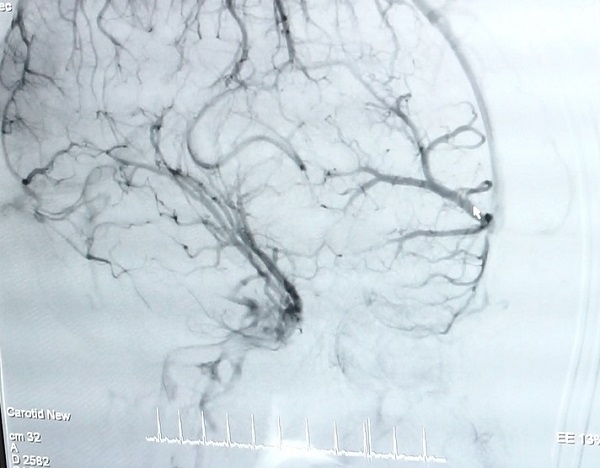
Clinical presentation (diagnostic event) was categorized as intracranial hemorrhage, proven by brain imaging, or seizure, focal neurological deficit, headache, or other event with signs of AVM hemorrhage on his brain imaging. March 22, 2019, MRI and CT-scan was performed at City International Hospital which revealed a extensive involvement of venous lesions and anomalies on the left temporal cerebral hemorrhage, A giant AVM was noted and definitely demonstrated on angiography performed by Dr. Tran Chi Cuong, senior consultant & Director of CIH-SIS Stroke Center,

Angiography performed by Dr. Tran Chi Cuong and his team
Described by Dr. Tran Chi Cuong, Clinically, Although relatively rare, their potentially devastating effects as a leading cause of hemorrhagic stroke in young individuals have raised their importance to a level that goes beyond what their epidemiology alone justifies. Arteriovenous malformations (AVM) are abnormal connections between arteries and veins and are usually present from birth and can cause brain hemorrhage later in life. AVMs in particular can be more serious diagnoses as they have the potential to cause debilitating symptoms, including the risk of rupture and bleeding into the brain.
Brain AVMs are an increasingly recognized cause of death and long-term morbidity, mostly due to intracranial hemorrhage and epilepsy; However, many patients who have experienced a brain hemorrhage do survive the initial event of an intracranial hemorrhage, with fast recovery and with extensive rehabilitation efforts, including physical, occupational, and speech therapy, patients can regain function.
With the advances in non-invasive imaging technology, visualization of AVMs (changes in the size, color or consistency of the lesion) became easier. Angiography was used to evaluate the angioarchitecture of the lesions, which includes number of AVMs, size and location of AVMs, origin and number of feeding arteries, location of draining veins, and occurrence of venous pouches.
A 28 year old male presenting with sudden onset of headache. A CT angiogram demonstrates a left frontal parenchymal haemorrhage
Angiography — Angiography is the gold standard for the diagnosis, treatment planning, and follow-up after treatment of AVMs Anatomical and physiological information such as the nidus configuration, its relationship to surrounding vessels, and localization of the draining or efferent portion of the AVM are readily obtained with this technique. Contrast transit times provide additional useful information regarding the flow state of the lesion; this is critical for endovascular treatment planning. Meaning it is important to recognize that when bleeding occurs within the brain itself. Incident AVM hemorrhage - a sudden and severe headache is a common symptom. Symptoms due to hemorrhage include loss of consciousness, sudden and severe headache, nausea, vomiting as the coagulated blood makes its way down to be dissolved in the individual's spinal fluid.
 The collective risk over one’s lifetime may be extremely high especially in a young person.
The collective risk over one’s lifetime may be extremely high especially in a young person.
Arteriovenous malformations (AVMs) are the most dangerous congenital vascular malformations. They have become the focus of scientific study leading to technological advances that have permitted these high-flow lesions to be treated, often with a multidisciplinary approach utilizing surgical, endovascular, and radiosurgical techniques. March 26, an improvement in the left hemiparesis and a reorganization of motor function were observed after endovascular treatment.

A multidisciplinary team that consists of a neurologist, an internist, neurosurgeon and invasive radiologist.
Dr. Tran Chi Cuong continued "Not all people who have AVMs will bleed during their lifetime. The risk is estimated to be about 4-6 out of every 100 people with an AVM will have a bleed during any given year. The collective risk over one’s lifetime may be extremely high especially in a young person. For instance, in a 50 year old with an AVM who has a life expectancy of 30 years, the risk of bleeding in his/her lifetime is >70%.. Risk factors can include high blood pressure and smoking. One thing that has been clearly shown is that symptomatic vascular masses that have bled in the past are at higher risk of bleeding again in the future. Seek immediate medical attention if you notice any signs or symptoms of a brain AVM, such as seizures, headaches or other symptoms. A bleeding brain AVM is life-threatening and requires emergency medical attention."
For appointment or more information about the services provided, please contact:
CIH-SIS Stoke Center (028) 6290.1155 or 18001115.
Patient service: (8428) 6280 3333, ext. 8535
- Address: Level 3, No. 3, 17A Street, Binh Tri Dong B Ward, Binh Tan Dist. (Next to AEON Mall Binh Tan). Ho Chi Minh City.
- Website: https://cih.com.vn/en/
- Email: This email address is being protected from spambots. You need JavaScript enabled to view it.